Real-world effectiveness of oral novel hormonal agents in patients with advanced prostate cancer: a head-to-head comparison using longitudinal, territory-wide electronic medical records
Yuanshi Jiao1, Isaac Ho2, Chunka Wong1, Tunghiu Li3, Jiaqi Wang3, Esther W Chan3, Xue Li1,3,*
ABSTRACT
Background
This study provided evidence addressing unreported direct comparison of effectiveness and health resource utilisation (HRU) of novel hormonal agents (NHAs) against chemotherapy for prostate cancer (PCa) for clinical decision-making.
Objectives
Evaluating the overall survival, prostate specific antigen (PSA) progression-free survival of adjunct treatments and their impact on HRU in a real-world context.
Methods
Design: A territory-wide, retrospective cohort study using electronic medical records (EMR) in Hong Kong.
Setting: EMRs data sourced from the Hong Kong Hospital Authority. The study population comprised patients diagnosed with PCa between 2001 and 2021. We include individuals prescribed any of the adjunct treatments: docetaxel, enzalutamide, or abiraterone. Patients were excluded if the diagnosis age was <40 years or had documented other malignancies.
Exposures: Two NHAs: abiraterone and enzalutamide. Chemotherapy: docetaxel.
Main outcome measures: The primary endpoint was overall survival. Secondary outcomes were PSA-PFS and annualised HRU during the follow-up period.
Statistical analysis: We employed propensity score matching in comparative analysis, based on 54 confounding factors. We implemented flexible parametric survival models based on preliminary analysis that indicated non-linearity in the hazard function to model overall and PSA progress-free survival. Further, we conducted inverse probability of treatment weighting and inverse probability of censor weighting for sensitivity analysis.
Results
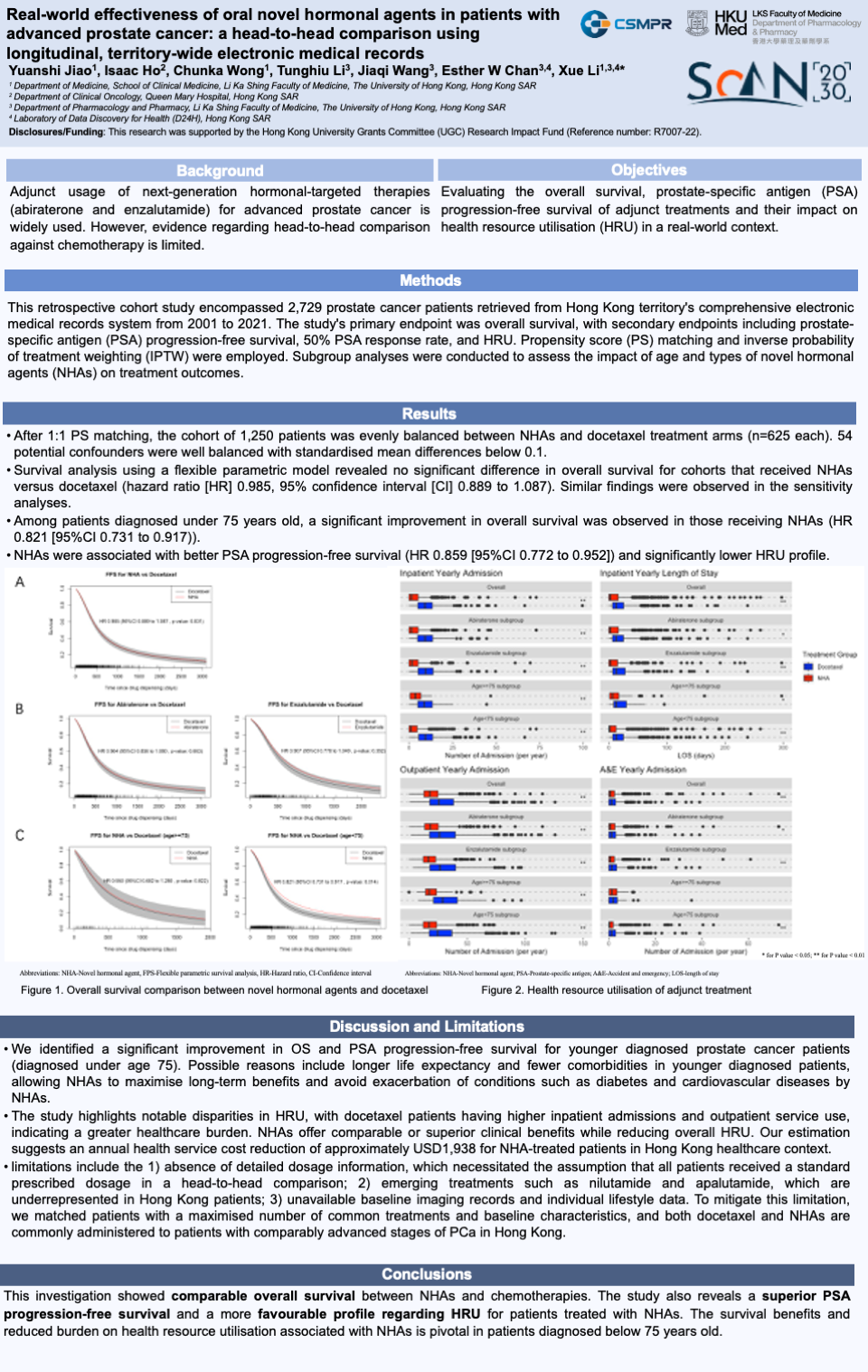
After PS matching, the cohort consisted of 1,250 patients evenly split between NHAs and docetaxel treatment arms (n=625 each). Survival analysis revealed no significant difference in overall survival for cohorts treated with both or either NHAs versus docetaxel (NHA: hazard ratio [HR] 1.02, 95% confidence interval [CI] 0.92 to 1.13, abiraterone: HR 1.04, [95% CI 0.93 to 1.17], enzalutamide: HR 1.10, [95% CI 0.95 to 1.29]) in line with sensitivity analysis. In patients diagnosed under 75 years, a significant improved overall survival was observed in those receiving NHAs (HR 1.22, [95% CI 1.09 to 1.37])
NHAs associated with better PSA-PFS (HR 1.16, [95% CI 1.05 to 1.30]). In HRU analysis, NHA treatments presented significantly lower health resource usage, evaluated by the median annual inpatient admissions numbered (NHA 1.37 [IQR: 0.00 to 5.14] vs docetaxel 9.04 [IQR: 4.98 to 13.28]), outpatient visits (NHA 17.73 [IQR: 12.75 to 24.90] vs docetaxel 25.70 [IQR: 17.74 to 38.21]), annual inpatient length of stay (NHA 2.44 days [IQR: 0.00 to 16.04] vs docetaxel 12.70 days [IQR: 6.33 to 25.41]).
Conclusions
Our findings showed a comparable overall survival between adjunct treatments but a superior PSA progression-free survival and HRU profile for NHAs.
1Department of Medicine, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR
2 Department of Clinical Oncology, Queen Mary Hospital, Hong Kong SAR
3Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR