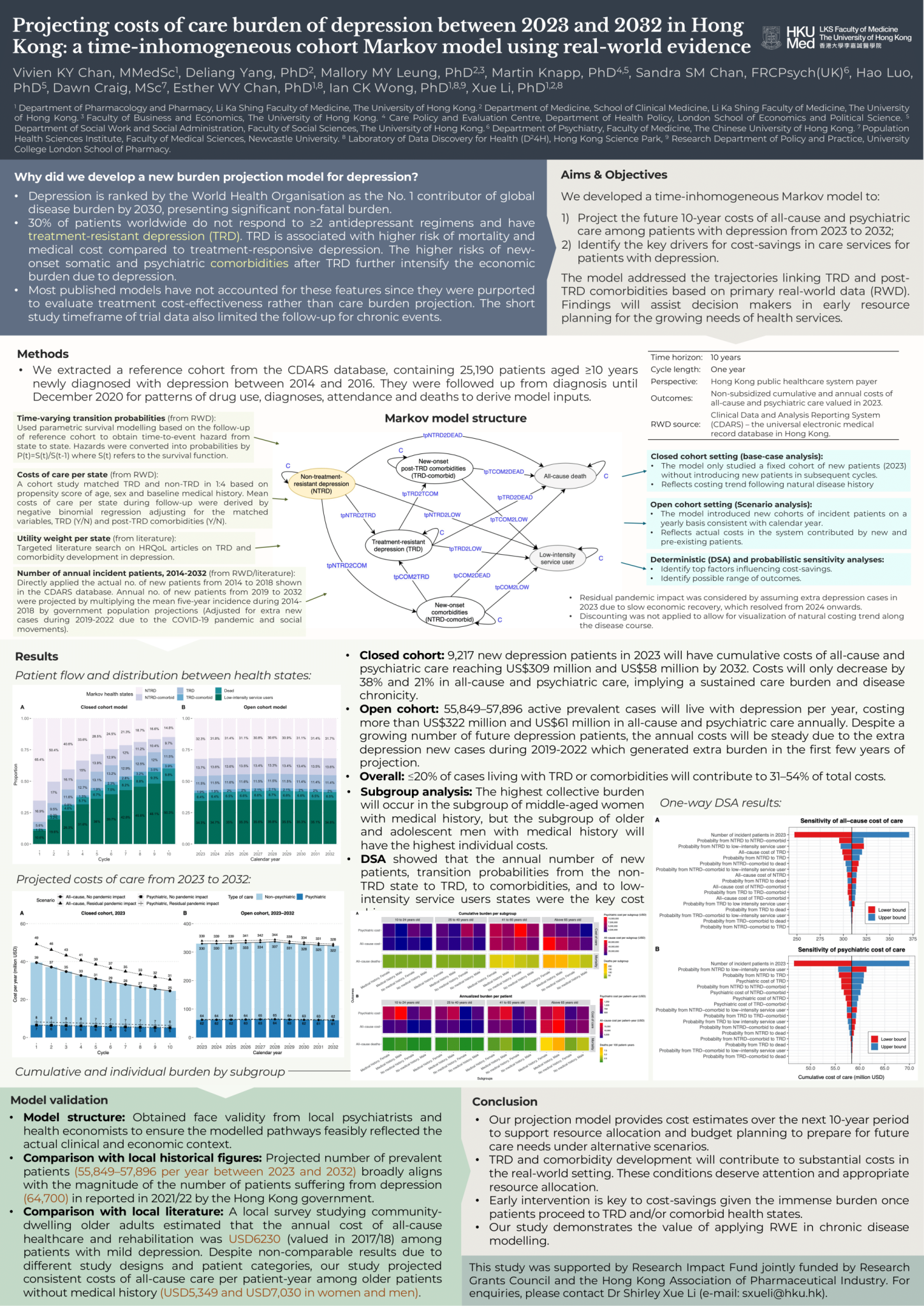
At the HTAi 2024 Annual Conference in Seville, I presented a poster on a 10-year projection model estimating the healthcare and mortality burden of depression in Hong Kong, using real-world patient data. By applying a Markov modelling approach, our study revealed that while fewer than 20% of patients develop treatment-resistant depression (TRD) or comorbidities, they account for over 30% of the healthcare costs. The findings highlight critical cost drivers in early disease stages and emphasize the value of leveraging real-world data to inform long-term resource planning and targeted policy interventions. Our real-world data validated that demographically-targeted policies are essential for equitable resource optimization in overburdened health systems.
Projecting the 10-Year Costs of Care and Mortality Burden of Depression until 2032: A Markov Modelling Study Developed from Real-World Data
Abstract
Background
Based on real-world data, we developed a 10-year prediction model to estimate the burden among patients with depression from the public healthcare system payer's perspective to inform early resource planning in Hong Kong.
Methods
We developed a Markov cohort model with yearly cycles specifically capturing the pathway of treatment-resistant depression (TRD) and comorbidity development along the disease course. Projected from 2023 to 2032, primary outcomes included costs of all-cause and psychiatric care, and secondary outcomes were all-cause deaths, years of life lived, and quality-adjusted life-years. Using the territory-wide electronic medical records, we identified 25,190 patients aged ≥10 years with newly diagnosed depression from 2014 to 2016 with follow-up until 2020 to observe the real-world time-to-event pattern, based on which costs and time-varying transition inputs were derived using negative binomial modelling and parametric survival analysis. We applied the model as both closed cohort, which studied a fixed cohort of incident patients in 2023, and open cohort, which introduced incident patients by year from 2014 to 2032. Utilities and annual new patients were from published sources.
Findings
With 9217 new patients in 2023, our closed cohort model projected the 10-year cumulative costs of all-cause and psychiatric care to reach US$309.0 million and US$58.3 million, respectively, with 899 deaths (case fatality rate: 9.8%) by 2032. In our open cohort model, 55,849-57,896 active prevalent cases would cost more than US$322.3 million and US $60.7 million, respectively, with more than 943 deaths annually from 2023 to 2032. Fewer than 20% of cases would live with TRD or comorbidities but contribute 31-54% of the costs. The greatest collective burden would occur in women aged above 40, but men aged above 65 and below 25 with medical history would have the highest costs per patient-year. The key cost drivers were relevant to the early disease stages.
Interpretation
A limited proportion of patients would develop TRD and comorbidities but contribute to a high proportion of costs, which necessitates appropriate attention and resource allocation. Our projection also demonstrates the application of real-world data to model longterm costs and mortality, which aid policymakers anticipate foreseeable burden and undertake budget planning to prepare for the care need in alternative scenarios.