The International Society for Pharmaceutical Engineering (ISPE) is a nonprofit association serving its members by leading scientific, technical, and regulatory advancement throughout the entire pharmaceutical lifecycle. Our abstract and poster of real-world comparative effectiveness study on prostate cancer treatment were presented in discussion sessions.
ABSTRACT
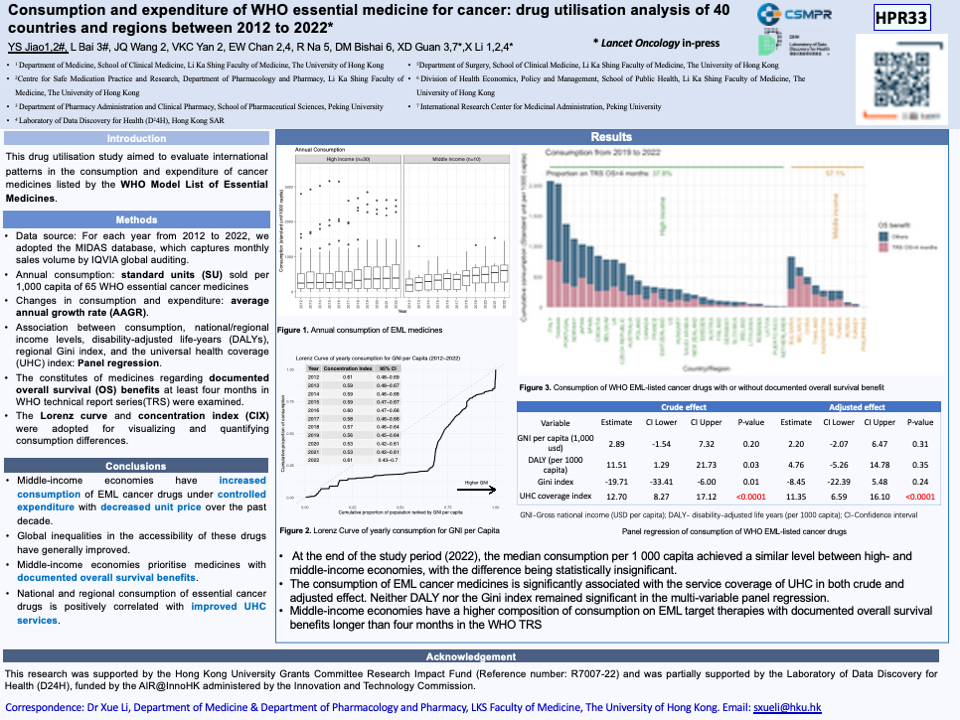
Consumption and expenditure of WHO essential medicines for cancer: drug utilisation analysis of 40 countries and regions between 2012 to 2022
Yuanshi Jiao1,2 #; Lin Bai3,#; Jiaqi Wang2; Vincent Ka Chun Yan2; Esther W Chan2,4; Rong Na5; David Makram Bishai6; Xiaodong Guan3,7*; Xue Li1,2,4,*
SUMMARY
Background
This drug utilisation study aimed to evaluate international patterns in the consumption and expenditure of cancer medicines listed by the WHO Model List of Essential Medicines.
Methods
We annualised consumption and expenditure data of 65 WHO essential cancer medicines between 2012 to 2022 from the MIDAS database, covering 30 high-, seven upper-middle-, and three lower-middle-income economies. Trends over the decade were assessed using rank-sum test, trends regression, and Lorenz curves. Panel regression assessed associations between consumption, country income levels, disability-adjusted life-years (DALYs) by neoplasm, Gini index, and the universal health coverage (UHC) index. The constitutes of medicines regarding WHO-documented overall survival (OS) benefits at least four months were examined.
Findings
By 2022, consumption of WHO essential cancer medicines (standard units per 1 000 capita) have no significant difference between high- and middle-income economies (median: 436.82 [Interquartile range (IQR): 92.66-800.14] vs 609.52 [IQR:278.44-762.50], p-value=0.84). Whilst per 1000 capita expenditure difference was evident (high-income: USD 133 198.82 [IQR:18 123.61-51 818.48], middle-income: USD 4 034.42 [IQR:2 502.68-5 805.27], p-value=0.0007). Over the 11 years, consumption (average annual growth rate: 16.8 [IQR:10.6-24.1]%) and expenditure (average annual growth rate: 9.0 [IQR:3.4-18.8] %) of WHO essential cancer medicines rapidly increased in the middle-income economies. UHC index is positively associated with consumption (coefficient: 11.35, 95% Confidence interval [CI]: 6.59-16.10, p<0.0001), while no significant effects have been observed with country income, DALYs or Gini index. Middle-income economies consumed more medicines with documented OS benefits over 4 months compared to high-income economies (57.1% vs 37.8 %, p=0.004).
Interpretation
Over the past decade, the consumption gap of WHO essential cancer medicines has narrowed among different economies, especially in middle-income economies. Improved UHC might improve treatment access. Middle-income economies prioritise medicines with documented survival benefits.
Funding
This research was supported by the Hong Kong University Grants Committee Research Impact Fund (Reference number: R7007-22) and was partially supported by the Laboratory of Data Discovery for Health (D24H), funded by the AIR@InnoHK administered by the Innovation and Technology Commission.
Keywords: WHO essential medicine; Cancer treatment; Drug Utilization; Healthcare expenditure; Accessibility; Health equality
1 Department of Medicine, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China. (YS Jiao MPH, X Li PhD)
2 Centre for Safe Medication Practice and Research, Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China (YS JIAO MPH, JQ Wang MSc, Prof EW Chan PhD, VK Yan PhD, X Li PhD)
3 Department of Pharmacy Administration and Clinical Pharmacy, School of Pharmaceutical Sciences, Peking University, Beijing, China. (L Bai MSc, XD Guan PhD)
4 Laboratory of Data Discovery for Health (D24H), Hong Kong SAR, China. (Prof EW Chan PhD, X Li PhD)
5 Department of Surgery, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China. (R Na, PhD)
6 Division of Health Economics, Policy and Management, School of Public Health, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China. (Prof DM Bishai PhD)
7 International Research Center for Medicinal Administration, Peking University, Beijing, China. (XD Guan, PhD)